
The Story
CMS has made its first changes to E&M coding in 20+ years. These changes modify the content of the medical note and how it relates to the E&M code that it translates to. The goal of this change was to eliminate the "note bloat" and complexity of code selection. CMS continues to refine these guidelines throughout 2021, creating additional uncertainty as hospitals' compliance and financial teams determine how the providers and/or coders handle these modifications. Without benchmarks to review, how do we know how our providers compare to their peers? Are they outliers? With 2021 Medicare comparison data not available until mid-2022, how do I proactively manage our physicians coding patterns?
REVEAL/md discussed these concerns with our clients and created an analytic that provides an opportunity for our clients to manage these changes proactively.
The Problem:
Compliance and Finance Officers
of Hospital System with 2,200 providers
With the documentation and coding changes in 2021 and the Pandemic affected data of 2020, how do we determine if our providers are on track or even changing their coding patterns due to the 2021 E&M documentation changes? How can we be proactive in managing risk and revenue opportunities without CMS comparative data? We can't wait until mid-2022 to determine if our providers are creating risk or potentially losing revenue for the organization.
The Approach:
- CMS lacks comparative data to compare 2021 E&M Changes: With the E&M documentation and coding modifications, Medicare will not have comparative data available until July 2022
- 2020 Pandemic does not show a true reflection of usual and customary practice patterns: A decision was made to disregard this data, for it was skewed due to COVID-19 lockdown and reduction in overall patient encounters.
- How do Finance and Compliance Teams stay proactive without comparable data? Upon investigation, it was decided that the proactive approach was to review physicians' own comparable data to determine shifts in coding patterns.
- Analyzed a hospital with 2,200 providers to determine if there was a shift in E&M coding: REVEAL/md started at the Organization level, then drilled down to region, specialty, and provider to determine the priority of provider reviews.
The Conclusion:
One Physician's RESULTS
2019 Compared to 2021
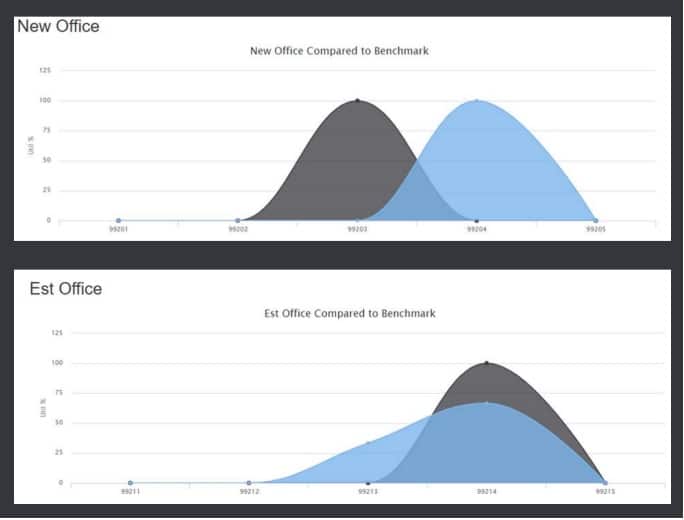
The two graphs on the left show actual physician data comparing the shifting patterns of the E&M visits for New and Established Office Visits from the benchmark 2019 data compared to January through May of 2021.
Looking at 2,200 providers' comparative data is essential in identifying potential risk or missed revenue opportunities. It is vital to review these coding shifts, or lack thereof, now before CMS comparative data is available in July of 2022 to remain proactive with your providers, coders, and insurance carriers.
With limited resources, it is critical to creating a winning game plan for chart reviews to ensure that documentation supports the services being billed and provides education as needed.
Enter your text here...
